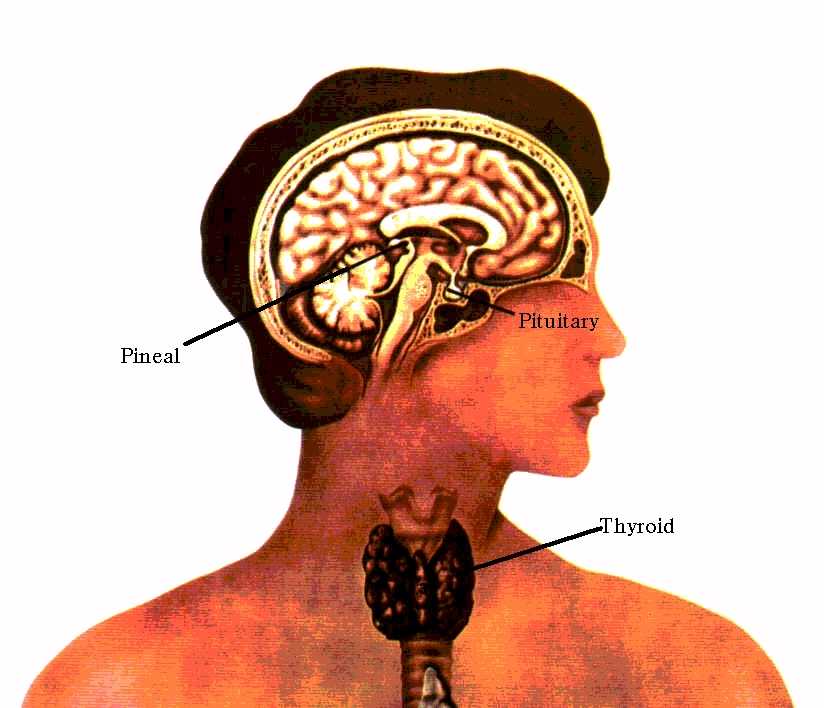
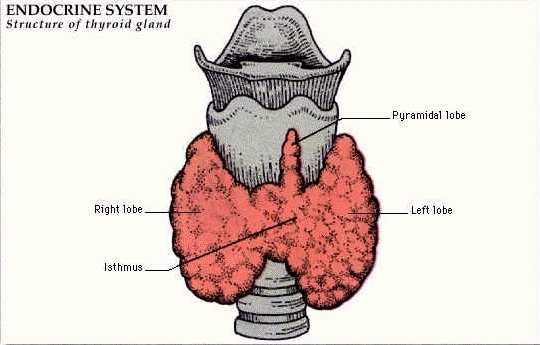
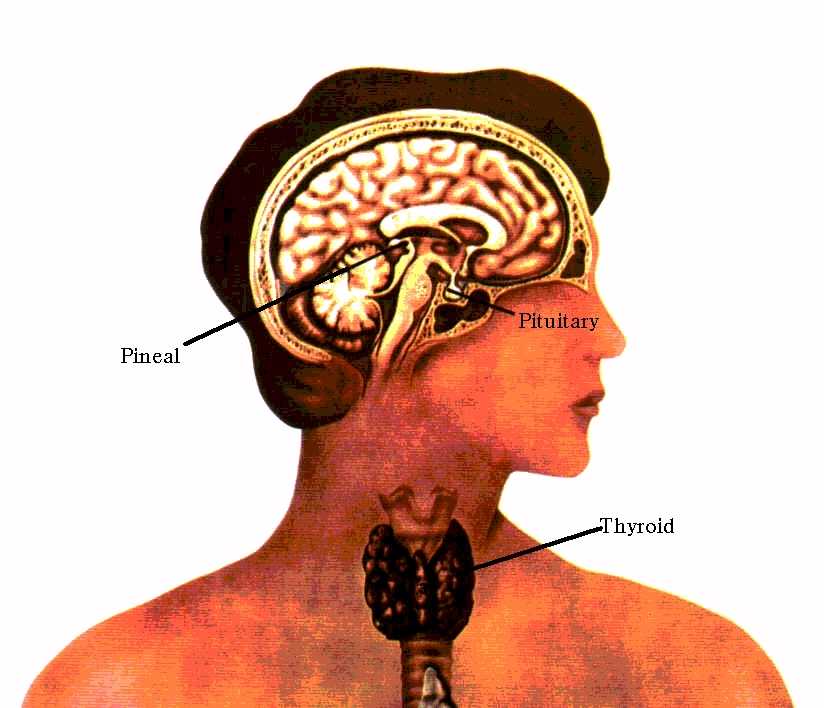
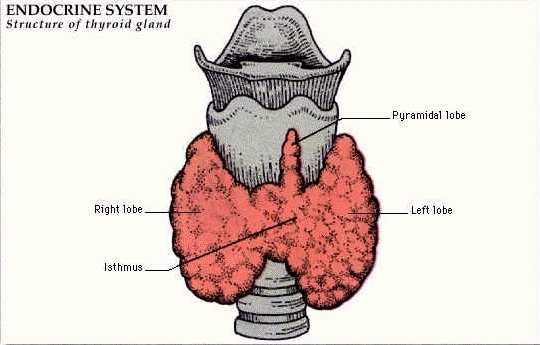
The thyroid gland is a butterfly shaped gland lying anterior to the trachea.
|
|
| Click on pictures for larger detail | |
The functioning unit of the thyroid is the follicle.
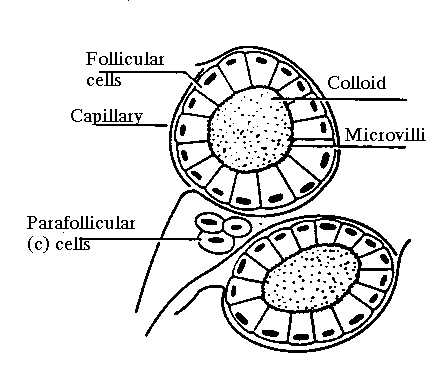
There are numerous follicles of varying sizes separated by connective tissue. ( Embedded in the connective tissue are parafollicular c-cells which produce calcitonin. )
Each thyroid follicle is spherical in shape and consists of a lining of epithelial cells surrounding a fluid called colloid. The base of each follicular cell lies adjacent to a capillary.
The thyroid produces two major hormones, thyroxine (T4) and triiodothyronine (T3).
It produces 100% of the T4 found in the body, and 20% of the T3. The other 80% of T3 found in the body is produced by peripheral conversion of T4 to T3.
T3 is the more active of the two hormones. It is the one which is responsible for the physiological response to thyroid hormone.
There are six steps involved in the production and release of the thyroid hormones:

a) Iodine from the diet is actively transported across the cell membrane.
b) The trapped iodine is transferred across the cell and into the colloid lumen where it is linked to tyrosine to for monoiodotyrosine (MIT) and di-iodotyrosine (DIT). These are contained within large proteins (thyroglobulin) which have been synthesized by the cells and sereted into the colloid.
c) While still linked to the thyroglobulin MIT and DIT are converted to T3 and T4 with the aid of the enzymes peroxidase and and transaminase.
d) T4 and T3, while linked to thyroglobulin, are reabsorbed into the cell in the form of colloid droplets.
e) T4 and T3 are separated from thyroglobulin.
f) T4 and T3 are secreted into the circulation. Any uncoupled MIT and DIT are deiodinated to release tyrosine and iodine which are then recycled.
Thyroid hormones in the circulation are bound to proteins, thyroxine binding globulin (TBG) and albumin.
TBG has a greater affinity for T4 than T3.
Albumin has a much lesser affinity for both hormones but binds a significant proportion of the hormones because it is present in greater proportions than TBG.
The synthesis and release of thyroid hormones is regulated by a negative feedback mechanism involving the pituitary hormone thyroid stimulating hormone (TSH) and the hypothalmic hormone thyrotropin releasing hormone (TRH).
Thyroid hormones affects nearly every cell and organ in the body.
- Regulate metabolic rate and growth
- Have an effect on many bodily mechanisms.
Examples:
synthesis of RNA and protein
stimulate certain enzyme systems
enhance release of free fatty acids from adipose tisssue
intestinal absorbtion and peripheral utilization of glucose.
At higher concentrations they decrease protein synthesis, increase the breakdown of glycogen, lipid and protein.
Symptoms of hypothyroidism and hyperthyroidism |
|
Hypothyroidism
|
Hyperthyroidism
|
|
| hair- dry, brittle | hair- thinning, fine |
| edematous eylids, ptosis | prominence of eyes, lid lag |
| puffy face, large tongue | |
| hoarseness, deepening voice | goiter |
| angina, decreased heart rate | palpitations |
| constipation | diarrhea, hyperdefecation |
| menorrhagia, dysmenorrhea in women | amenorrhea, decreased menstrual flow in women |
| brittle nails | palmar erythema |
| cold, dry, yellowish skin | hot, flushed, moist skin |
| muscular pain, weakness | muscular fatigue, weakness |
| cold intolerance | heat intolerance |
| decreased sweating | increased sweating |
| lethargy | nervousness |
| tiredness, fatigue | irritability, insomnia |
Ultrasensitive hTSH II is the most sensitive test we currently have.
This new test differs from the old one in that it can detect abnormal levels (too high or too low) in the presence of normal T4 and T3 values.
The TRH stimulation test used to make the differential diagnosis between primary hypopothyroidism and secondary hypothyroidism.
| a) Primary Hypothyroidism | b) Secondary Hypothyroidism | c) Hypothalamic Hypothyroidism |
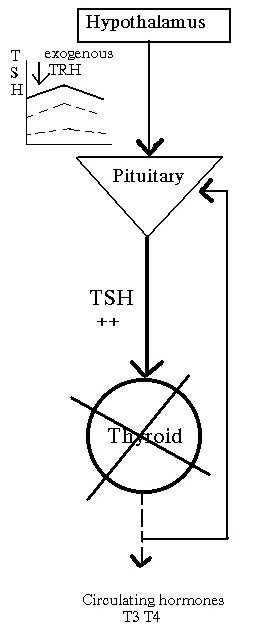 | 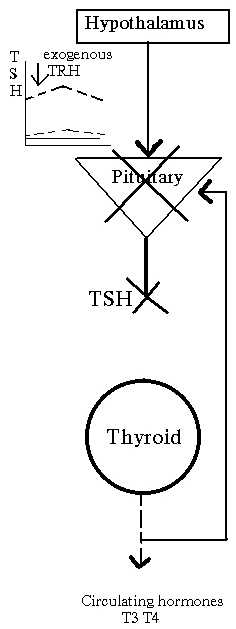 |  |
| T4 low, TSH response exaggerated | T4 low, No TSH response | T4 low, Delayed TSH response |
By employing this supersensitive test we can detect subclinical thyroid disorders which we can then treat.
Two reasons for treating subclinicak hypothyroidism are:
1) 5% of younger patients and 20% of older patients annually will convert from subclinical to overt hypothyroidism.
2) Reverse any negative effects at the tissue level- i.e.
liporprotein fraction.
Causes of hypothyroidism
- iodine dificiency
- auto immune thyroditis
Hashimoto's thyroditis- a chronic inflammation of the thyroid. probably the most common cause of hypothyroidism. occurs more frequently in women
(8:1), between the ages of 30-50. A family history of thyroid disorders is common.
- post surgery
- post radio-iodine therapy
- acute thyroditis
an acute inflammatory disease probably caused by a virus. frequently there is a history of mumps. has been discribed following a variety of upper
respiratory tract inffections. self limiting, but rarely results in hypothyroidism.
- silent thyroditis
post-partum thyroditis- a subacute disorder in the post-partum period. usally a self limiting period of hyperthyroid phase of several weeks to several months, often followed by transient hypothyroidism with eventual recovery.
- pituary or hypothalamic disease
- drugs
Amiodarone: an antiarhythmic drug which is structurally similar to thyroid hormones and contains a significant amount of iodine. it interferes with the peripheral conversion of T4 and T3. 10-15% of patients on Amiodarone become hypothyroid.
Iodine: elevated concentrations may inhibit synthesis and release of T4 and T3 in susceptible patients. Rare
Lithium: can block the release of thyroid hormones from the thyroid gland. Occurs in 5-15% of patients on long term therapy.
Thyroid hormone replacement agents availible: