Inflammatory Bowel Disease
Prepared by: Eric Brandt, B.Sc. Pharm
Inflammatory Bowel Disease is a general term used to describe two chronic inflammatory diseases occurring primarily in the gastrointestinal tract; Ulcerative Colitis and Crohn's Disease
Epidemiology
Ulcerative Colitis and Crohn's disease share many epidemiologic features
more common in western societies
higher incidence among Jews of Eastern European descent
low frequency among non-whites
both sexes affected equally
usually affect people before the age of 40
tend to occur in the same families
in Western Canada the prevalence is three times the global one, 150 per 100,000 Vs 50 per 100,000
Etiology
unknown
theories of possible etiology include:
- infectious agents- no causative bacteria has been cultured, bacterial overgrowth seen is probably due to favorable environment rather than relevant to pathogenesis
- genetic factors- the increased frequency in whites, Jews, and family members is suggestive of genetic predisposition, but no genetic marker has been identified.
- immunologic mechanisms
- allergic reaction to cows' milk
- imp
aired cellular immune mechanisms
- hypersensitivity reaction
- autoimmune antibody mediated reaction, suggested by extra intestinal manifestations and the fact that treatment with corticosteroids leads to favorable response.
- psychological factors- no proof that stress causes the disease but psychological factors may influence the course of the disease.
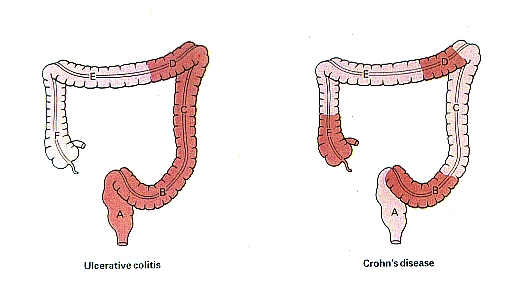
Important differences between Ulcerative Colitis and Crohn's Disease
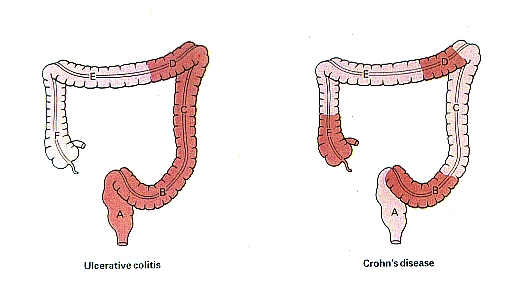
- Incidence of Ulcerative Colitis is static; Crohn's is increasing.
- Only the colon is affected in Ulcerative Colitis; Crohn's can also affect the small bowel
- Ulcerative Colitis has a marked tendenct to relapse and remit; Crohn's is similar but less marked.
- Clinical features of abdominal mass, signs of malabsorption, fistula formation and gross perianal disease do not occur in Ulcerative Cilitis
- deep Radiological features- Ulcerative Colitis changes affect rectum and proximal colon in continuity; fissuring and aphthoid ulceration, 'skip' lesions and small bowel involvement are features of Crohn's Disease.
- Histological features- transmural inflammation, fissuring granulomas and goblet cell preservation are features of Crohn's Disease, Ulcerative Colitis is characterized by mucosal inflammation, crypt abscesses and goblet cell depletion.
Treatment goals
- terminating an acute attack and inducing remission
- preventing relapse
- controlling chronic symptoms
Treatment is individualized and includes drugs, nutritional support, and if necessary surgical intervention.
DRUGS
Anti-inflammatories
Sulfasalazine
- 20 % absorbed
- remainder goes to the colon where colonic bacteria cleave the diazo bond to liberate the 5-ASA
- the sulfapyridine is then absorbed and excreted in the urine
- the 5-ASA molecule remains in the colon where it exerts its actions as local anti-inflammatory
- adverse effects are associated with the sulfapyridine molecule and include nausea, malaise, headache, anorexia, hypersensitivity reaction, vomiting, dyspepsia
Corticosteroids
available in several forms; oral, injectable, enema
considered drugs of choice in the treatment of acute severe attacks and exacerbations
more immediate response than sulfasalazine
Immuno Suppresive Agents
- Azathioprine
- 6-mercaptopurine (6-MP)
- Bacillus Calmette-Guerin (BCG)
- Levamisole
- Transfer factor
not for ulcerative colitis
limited to patients with refractory Crohn's Disease who require high prolonged doses of steroids to control their symptoms and because of the extent of their disease surgery is precluded.
Antimicrobials
Metronidazole
no evidence of effectiveness in Ulcerative Colitis
may be effective in some Crohn's patie.ts who fail to respond to Sulfasalazine
Antimotility agents
- Diphenoxylate
- Loperamide
- Codeine Phosphate
- Tincture of opium
- Tincture of belladonna
- Cholestyramine (bile salt binding)
- Hydrophyllic compounds (Psyllium)
Mast cell stabilizers
Cromolyn sodium
Investigational drugs
- Nicotine patch
- Leukotriene inhibitors